Lipitor's Potency: How It Measures up Clinically
Atorvastatin frequently behaves like a heavyweight in trials, delivering marked LDL-C reductions compared with other statins. Large randomized studies and meta-analyses demonstrate dose-dependent potency, which physicians translate into lower rates of heart attacks and strokes in higher-risk patients.
Clinicians balance potency with tolerance: stronger LDL lowering can mean higher adverse event signals, but most side effects remain uncommon. Population data and head-to-head trials help predict who will gain the greatest benefit, and a switch or dose change may be wiser.
This view blends numbers and narrative — explaining why choosing a more potent statin may be decisive for some and unnecessary for others. Occassionally clinicians weigh patient preference and prior experiance to accommodate individual goals.
| Measure | Atorvastatin vs Others |
|---|---|
| LDL reduction | Higher at equivalent doses |
| CV outcome | Robust evidence of risk reduction |
Side Effects Showdown: Muscle, Liver, and Diabetes Risk

Patients often describe muscle aches when starting statins, and clinicians must distinguish benign myalgias from true myopathy. lipitor is associated with low rates of severe muscle injury, but higher doses raise the risk and monitoring is prudent.
Liver enzyme elevations occur infrequently; baseline tests and follow-up can detect clinically relevant changes. Occassionally transaminases rise but usually normalize with dose adjustment or switching agents — serious hepatic failure is rare across statins.
Patients with diabetes risk factors should discuss evidence that statins slightly increase diabetes incidence, especially at higher intensity, balanced against robust cardiovascular benefit. Personalized choice, shared decision-making, and regular review help acheive optimal outcomes. Clinicians monitor glucose and tailor therapy according to overall risk.
Cholesterol Lowering Speed and Long Term Outcomes
When a person begins statin therapy, LDL levels often fall noticeably within a few weeks; early responses are faster with more potent drugs such as lipitor.
Most patients reach a near-maximal reduction by about one month, with additional small gains over subsequent months. Large randomized trials then link those biochemical gains to fewer heart attacks and strokes over years.
Comparisons show that larger initial LDL drops generally predict greater relative risk reduction, but absolute benefits accumulate over long follow-up. Adherence and lifestyle are major modifiers of that trajectory.
Clinicians therefore weigh the need for rapid control against tolerability and safety, titrating dose or switching agents if goals arent met. Definately, long-term monitoring transforms early promise into sustained cardiovascular protection. Elderly patients and those with diabetes may need individualized strategies and more frequent follow-up to ensure benefit and safety monitoring regularly.
Drug Interactions and Real World Prescribing Considerations

Prescribers often narrate a familiar scene: a patient juggling blood thinners, diabetes meds and supplements while seeking better cholesterol control. Lipitor (atorvastatin) is metabolized by CYP3A4, so potent inhibitors like certain antifungals or macrolides can elevate levels and muscle toxicity risk. Occassionally grapefruit juice compounds this effect; clinicians must reconcile interactions with real-world polypharmacy.
In practice, warfarin, fibrates and certain immunosuppressants alter statin risk profiles, and renal or hepatic impairment shifts choice and dose. Older adults with polypharmacy require close review, baseline LFTs and CK when symptoms arise, and clear plans for monitoring. Good prescribers weigh evidence, patient goals and access to generics while using shared decision-making to acheive safe, effective therapy and reliable follow-up.
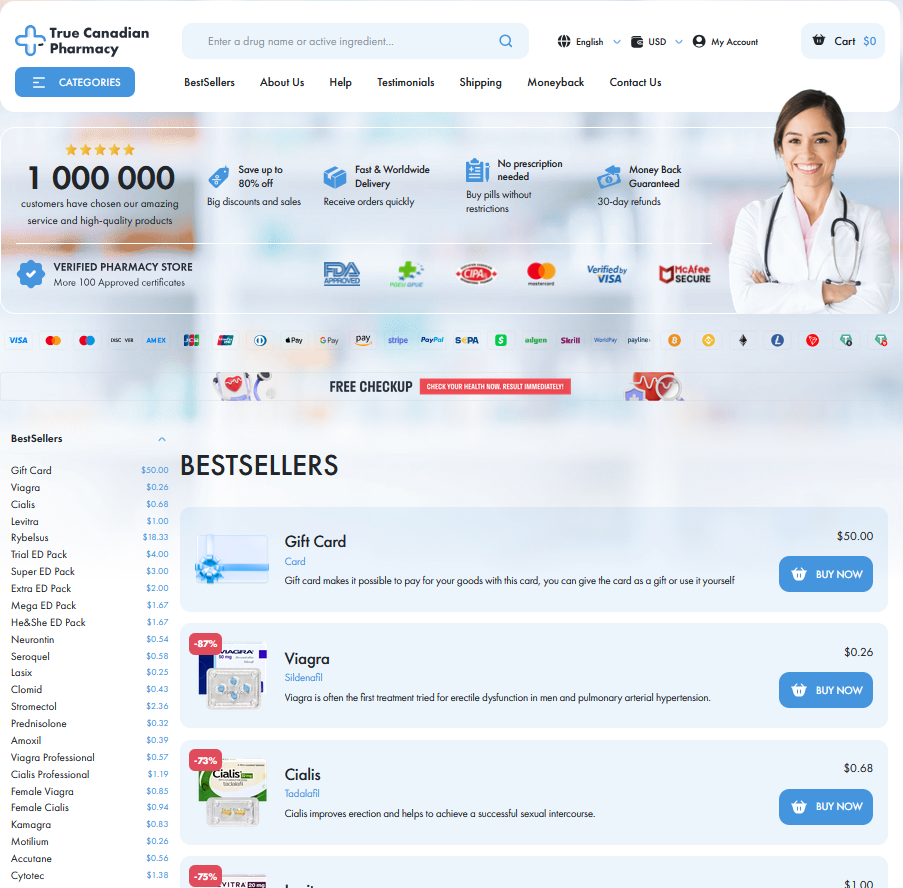
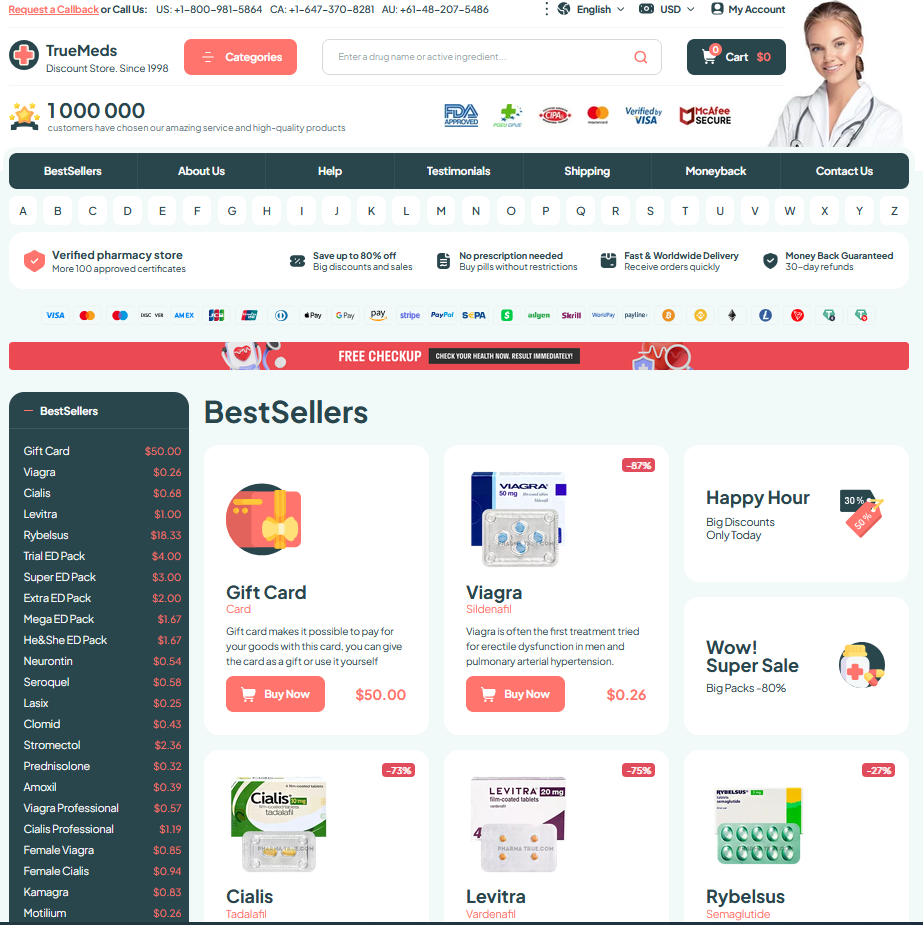
Cost, Generics, and Accessibility Across Populations
Affordability shapes who receives high-potency therapy and how quickly clinicians escalate treatment. When high doses are required, brand-name lipitor once set the market tone; generics shifted access, making therapy attainable for many and reducing therapy delays that can affect outcomes.
Insurers, pharmacy benefit managers, and national formularies drive which statin is favored. Copays and prior authorization can push clinicians toward cheaper alternatives or keep patients on older meds. In low-resource regions, program support and tiering determine whether people recieve evidence-based prevention.
Practical access varies: clinic stocking, subsidies, clinician comfort, local guidelines, pharmacy supply chains, and transportation barriers all influence prescribing, refill continuity, patient adherence, and equity over time across systems.
| Type | Typical monthly cost |
|---|---|
| Lipitor (brand) | $150+ |
| Generic atorvastatin | $10–30 |
Personalized Choice: Tailoring Statin Therapy by Patient
Imagine a patient entering clinic with a family history of heart disease who worries about side effects. Clinicians weigh age, baseline LDL, cardiovascular risk, liver and muscle history, diabetes or CKD, medication burden and pregnancy plans to decide whether Lipitor’s potency is appropriate or a different statin or dose suits better. Genetic factors, prior response patterns and patient values also shape the choice; providers occassionally use pharmacogenetic data or trial-and-error to guide therapy.
The plan may favor high-intensity atorvastatin for rapid LDL reduction or a moderate statin for frail, polypharmacy or preference-driven cases, paired with monitoring of LFTs and CK and symptom counselling. Shared decision-making, affordability and review improve adherence and acheive long-term risk reduction. NCBI StatPearls - Atorvastatin FDA Label - Atorvastatin (Lipitor)