Understanding Amoxil's Mechanism of Action
Amoxil, commonly known as amoxicillin, operates primarily by inhibiting the synthesis of bacterial cell walls. When bacteria are unable to build sturdy cell walls, they become susceptible to external pressures and eventually burst, leading to their demise. Amoxil specifically targets the penicillin-binding proteins located inside the bacterial cell wall, disrupting the assembly of peptidoglycan, a critical component for bacterial rigidity and strength.
The antibiotic's action spectrum is broad, meaning it can combat a wide range of bacterial strains, making it extremely versatile in clinical settings. Infections ranging from respiratory issues to skin infections can often be tackled by Amoxil, thanks to its effective penetration capabilities.
One remarkable feature is its ability to be absorbed quickly when taken orally, making it highly convenient for patients compared to some other antibiotics requiring intravenous administration. Furthermore, Amoxil's relatively simple mechanism of action allows healthcare providers to prescribe it confidently, knowing its predictable and robust effects.
| Characteristic | Details |
|---|---|
| Mechanism | Inhibits bacterial cell wall synthesis |
| Spectrum | Broad-spectrum |
| Absorption | Quick oral absorption |
| Convenience | Often preferred for its ease of use |
Comparing Efficacy: Amoxil Vs. Other Common Antibiotics

Amoxil, a penicillin-class antibiotic, is frequently prescribed due to its successful outcome in treating various bacterial infections. Its effectiveness largely stems from its mechanism of action, which inhibits bacterial cell wall synthesis, rendering bacteria unable to survive. When compared to antibiotics like azithromycin and ciprofloxacin, Amoxil holds its own, particularly against gram-positive bacteria.
However, antibiotics such as azithromycin excel against certain atypical pathogens, making them more suitable in specific scenarios like respiratory infections. Despite this, Amoxil's broad-spectrum nature allows it to treat a wider array of infections, including ear, nose, throat, and urinary tract infections, providing a versatile option in the medical arsenal.
Side Effects: How Amoxil Stacks up
Amoxil, a widely prescribed antibiotic, commonly causes mild side effects such as nausea, diarrhea, and skin rash. These typically resolve on their own and don't require medical intervention. However, when comparing Amoxil to other antibiotics like ciprofloxacin or azithromycin, it tends to have a lower incidence of severe side effects such as tendonitis or QT prolongation. This makes Amoxil a preferred option for many, especially in outpatient settings, where mitigating potential adverse reactions is crucial for patient compliance and comfort.
Treatment Scope: Broad Vs. Narrow-spectrum Antibiotics

Amoxil falls under the category of broad-spectrum antibiotics, capable of targeting a wide array of bacterial infections. This characteristic makes it highly versatile in treating various ailments, from respiratory infections to urinary tract infections. However, this broad reach can also disrupt beneficial bacteria, potentially leading to side effects like gastrointestinal upset.
On the other hand, narrow-spectrum antibiotics target specific types of bacteria, minimising collateral damage to the body's beneficial microbiome. These antibiotics are particularly useful in targeted treatments where the bacterial culprit is already identified. Narrow-spectrum alternatives are generally associated with fewer side effects, but require accurate diagnosis for effective use.
When comparing Amoxil's broad-spectrum capabilities to narrow-spectrum antibiotics, it's essential to balance efficacy against potential drawbacks. While Amoxil offers robust initial treatment options, overuse can contribute to antibiotic resistance, prompting some practitioners to reserve it for cases where narrow-spectrum options are ineffective.
Antibiotic Resistance: the Challenge of Amoxil
Antibiotic resistance is a mounting concern, and Amoxil, like other antibiotics, faces this formidable challenge. Overuse and misuse of Amoxil can lead to bacterial mutations, rendering the drug less effective over time. For instance, while Amoxil is highly effective against various strains of bacteria initially, repeated exposure allows for resistant strains to emerge.
Bacterial resistance not only diminishes Amoxil's efficacy but also complicates treatment protocols, necessitating alternative or more potent antibiotics. This issue emphasizes the need for judicious use of Amoxil to preserve its effectiveness. As healthcare providers confront the growing problem of resistance, adherence to proper dosage and treatment duration becomes critical.
Additionally, public awareness campaigns are essential to educate patients on the perils of incomplete antibiotic courses. With concerted efforts from both medical professionals and patients, the spread of resistant strains can be mitigated. Understanding the balance between effective treatment and resistance management is crucial for maintaining the long-term viability of Amoxil.
| Aspect | Details |
|---|---|
| Effectiveness | Initially effective, but can face resistance over time |
| Challenges | Management of resistant bacterial strains |
| Solutions | Proper use, adherence to dosage, public awareness |
Cost and Availability: Amoxil Compared to Alternatives
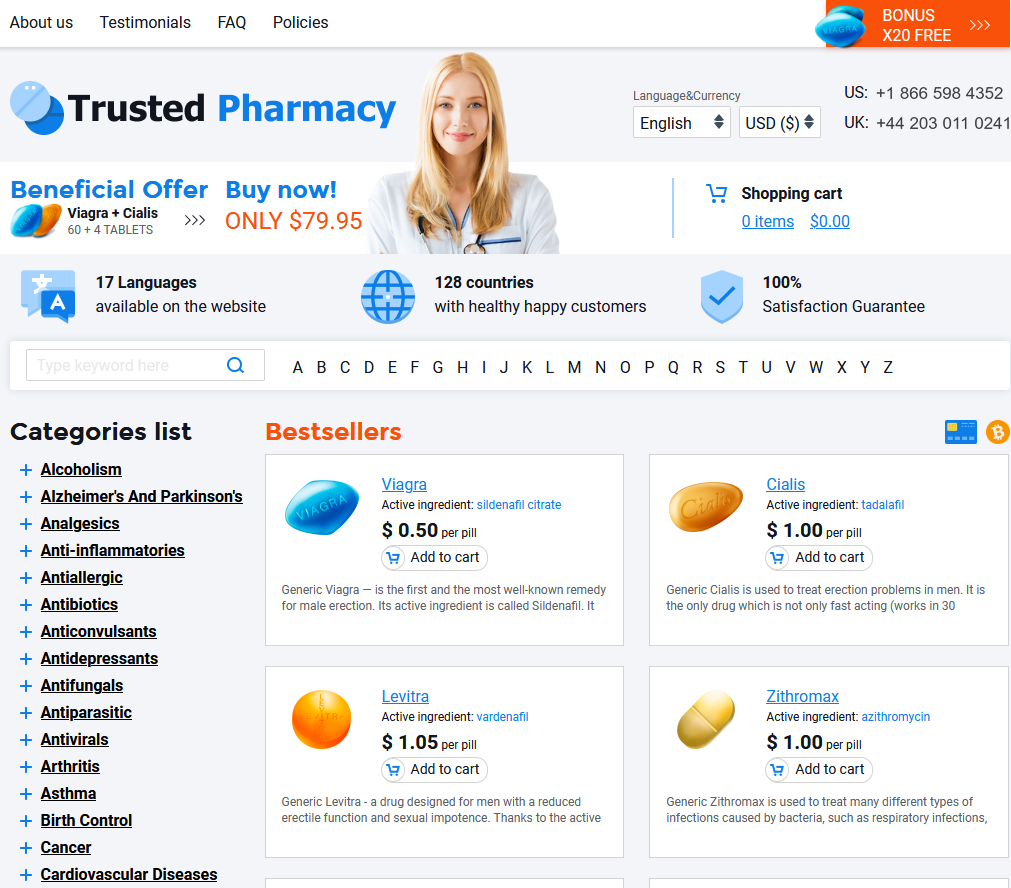
When it comes to the financial aspect of treatment, Amoxil often stands out due to its cost-effectiveness. Generally, Amoxil is more affordable than many other antibiotics on the market, making it a popular choice for both healthcare providers and patients. Availability is another strong suit for Amoxil; it is widely accessible in most pharmacies, ensuring that patients rarely encounter difficulties in obtaining it.
However, cost and availability can vary depending on the region and healthcare system. While some newer or more specialized antibiotics might offer advanced features, they often come at a higher price. Thus, in terms of accessibility and affordability, Amoxil remains a favorable option.